The future of the ACA was uncertain throughout 2017, and though President Trump recently took steps to dismantle it via executive order, it remains unclear how, and how soon, his actions will affect healthcare.
It should come as no surprise then that, according to Managed Healthcare Executive's 2017 State of the Industry Survey, government requirements and mandates top your list of challenges. In addition, shifting toward value-based care is high on the list, as is using big data to improve healthcare quality and reduce healthcare costs. Controlling rising specialty drug costs is another big burden.
The survey's findings, based on more than 300 responses received during the third quarter of the year, show the biggest challenges that executives at health systems, health plans, pharmacy benefit organizations, and more are facing and anticipate continuing to face next year. Here's a closer look at the survey results, and what industry experts advise organizations to do to overcome these challenges.
Challenge #1: Complying with government requirements and mandates
Adhering to government requirements and mandates tops all challenges, at a whopping 34%. This is down just a tad from last year's survey, when it was 36%. "The big question on everyone's mind is, what will become of the ACA?" says Zach Hafner, national partner, consulting, Advisory Board, a healthcare consultancy firm. "Addressing this question at this point requires more precision because the government is deconstructing the broader legislation and taking on various components of it."
President Trump recently announced he will end cost sharing reduction payments to insurers, and he scaled back requirements for employers to provide birth control as part of health coverage for employees. "But these aren't the only potential targets; pre-existing conditions, mandatory insurance coverage, minimum policy inclusions, Medicaid expansion, and selling health insurance policies across state lines are all potential pressure points as the law is revisited and revised in the coming year," Hafner says.
Challenge #2: Implementing value-based reimbursement
Placing second among survey respondents' biggest challenges is implementing value-based reimbursement, which received 22% of responses. Overall, more than half of survey participants, 56%, either have not yet started value-based payment initiatives or have only started a few initiatives. This does show some progress, as last year nearly 70% of survey respondents said they had not yet started or only had a few initiatives started.
Hafner says one reason organizations struggle in this area is that today's fee-for-service system is not well aligned to deliver true value-based care, and for most provider and payer participants, most business remains fee-for-service. The country continues to tolerate fee-for-service and annual reimbursement increases. "Until that changes, we can't really expect payers and providers to make the change," he says.
Secondly, delivering value-based care requires different infrastructure, work flow, and information than what has been in place historically, all of which require investment. Some examples of this include physicians needing to collaborate, integrating clinical and financial data, and having the capability to evaluate, negotiate, and administer risk-based contracting arrangements. To date, the return on such investments has been elusive.
Thirdly, even after a decision is made to move a business model to value-based pay, data and insights needed are not easy to obtain and often considerable lag time occurs when compiling it.
Challenge #3: Using big data to improve quality and reduce costs
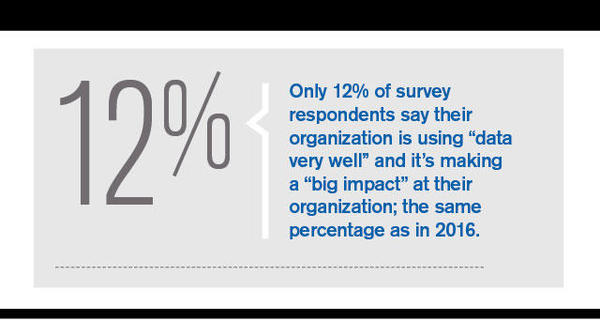
This is a third major challenge facing organizations. Only 12% of survey respondents say their organization is excelling in this area; the same percentage as in the 2016 survey. Forty six percent of 2017 survey respondents say they "have come a long way" in this area, but that they have a lot more work to do in this space. That's up from 39% last year.
Shroff sees two main big data challenges. Although more healthcare data is being generated, the data is scattered across multiple entities--payers, providers, and patients. There is no such thing as a single "source of truth" for healthcare data.
"When patients jump between different health plans or providers, the data doesn't follow the patient," he says. "This, coupled with the lack of interoperability between entities, makes it difficult to harness data-driven insights."
Secondly, most organizations lack the proper technology to manage or capitalize on the vast amount of information they possess. Healthcare data comes in various formats and sources--clinical data from EHRs, billing data from claims, patient enrollment or registration data, as well as self-reported patient data, Shroff says. To truly unlock the power of big data, organizations need a technology infrastructure that retrieves, stores, and analyzes various sources of data at scale.
Health plans and systems have the same challenge--getting access to the data that the other has. "A health system has access to the patient's most in-depth clinical data, but it's often limited to the specific episode of care that was provided at that system," Shroff says. "When a patient visits other provider groups or hospitals, it's the patient's responsibility to recall the care that was provided at the other settings." On the other hand, health plans are aware of every encounter that a patient has, regardless of which system they visit. However, their depth of knowledge is limited to the billing data sent from the systems. "Having both entities share their respective data would most likely result in better quality and cost savings, but organizations are simply not set up to do so in today's world."
Source: Modern Medicine Network (View full article)
Posted by Dan Corcoran on January 10, 2018 07:13 AM


Post a comment